GENERAL MEDICINE -A 70 year old male
is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
Chief complaint:70 year old male patient came to OPD with chief complaint of loss of speech since one day
History of present illness:patient was asymptomatic one month ago then he had fever nd chills not associated with nausea, vomiting,loose stools.Investigations were done diagnosed with pulmonary tuberculosis deranged lft , anti tubercular drugs were prescribed and discharged
Patient came to follow up to hospital 2days ago he was prescribed new medication due to deranged lft rft
Since last evening 6pm he had loss of speech
No loss of movements in upper and lower limbs
No mouth deviation
No history of epilepsy
No history of sob
No history of burning micturition
No history of nausea, vomiting,loose stools
History of past illness
K/c/o of pulmonary tuberculosis
K/c/o of hypertension
No history of diabetes,CAD
Personal history
Appetite -lost
Diet-mixed
Bowels-constipation
(Stools once in 2-3 days)
Micturition -decreased urine
Additions-alcohol 90ml/day since 35 years
Tobacco-one cigar 2-3 per day
Family history No revelant family history
General examination
Patient is conscious incoherent non cooperative
Not well oriented time place and person
Weekly built
No pallor
Icterus-present
No cyanosis
No clubbing
No edema
No lymphadenopathy
Vitals
Temperature -afebrile
Bp-90/60mmhg
Pulse rate-72bpm
Respiratory rate-10 cycles per minute
Systemic examination
Cvs-s1 s2 (+) no murmurs heard
CNS
Speech-loss of speech
Behaviour-involuntary movements of hands
Memory-not able to recognise family members
Motor examination -right. Left
UL. LI. UL. LI
Tone-decreased decreased
Power-decreased. Decreased
Reflexes:right. Left
Biceps-. 2+. 2+
Triceps-2+. 2+
Knee-2+. 2+
Ankle-2+. 2+
Sensory examination
Spinothalamic tract:right. Left
Pain. Absent. Absent
Temperature. Normal. Normal
Posterior column:
Fine touch. Absent Absent
Examination of respiratory system
Shape of chest -symmetrical
Chest expansion equal on both sides
Trachea is in central position
No scoliosis
Percussion:dullness on percussion
Auscultation:vesicular breath sounds
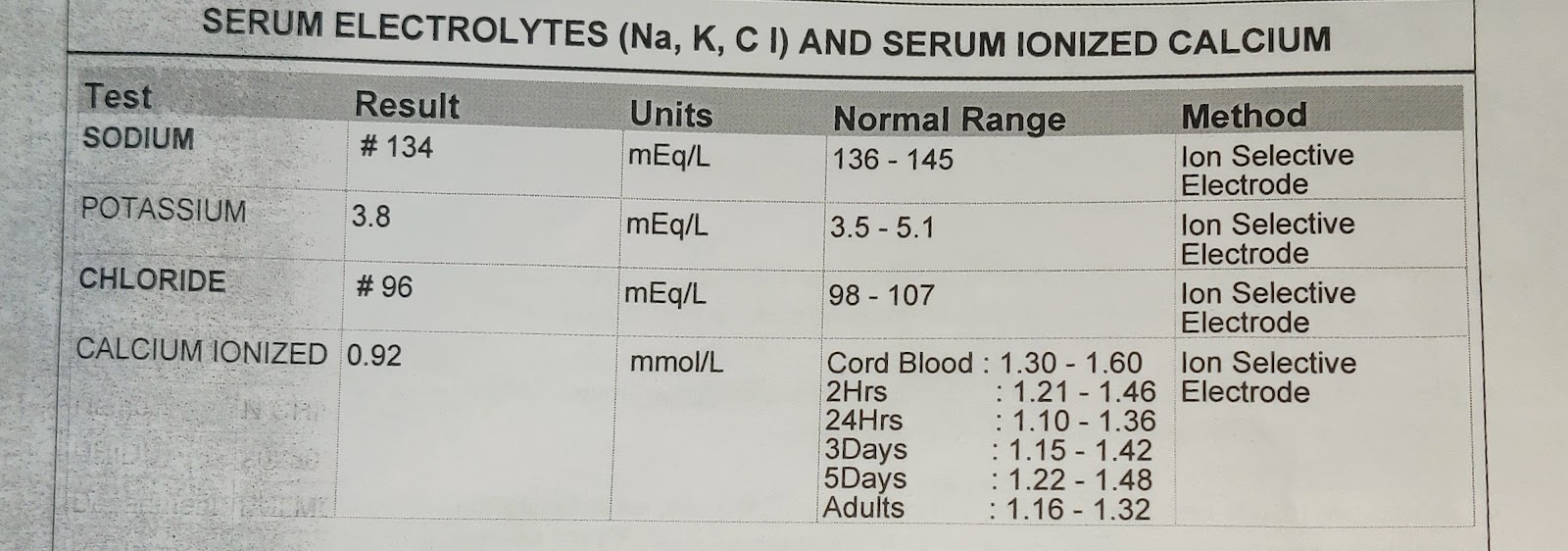
Investigation :
Treatment:
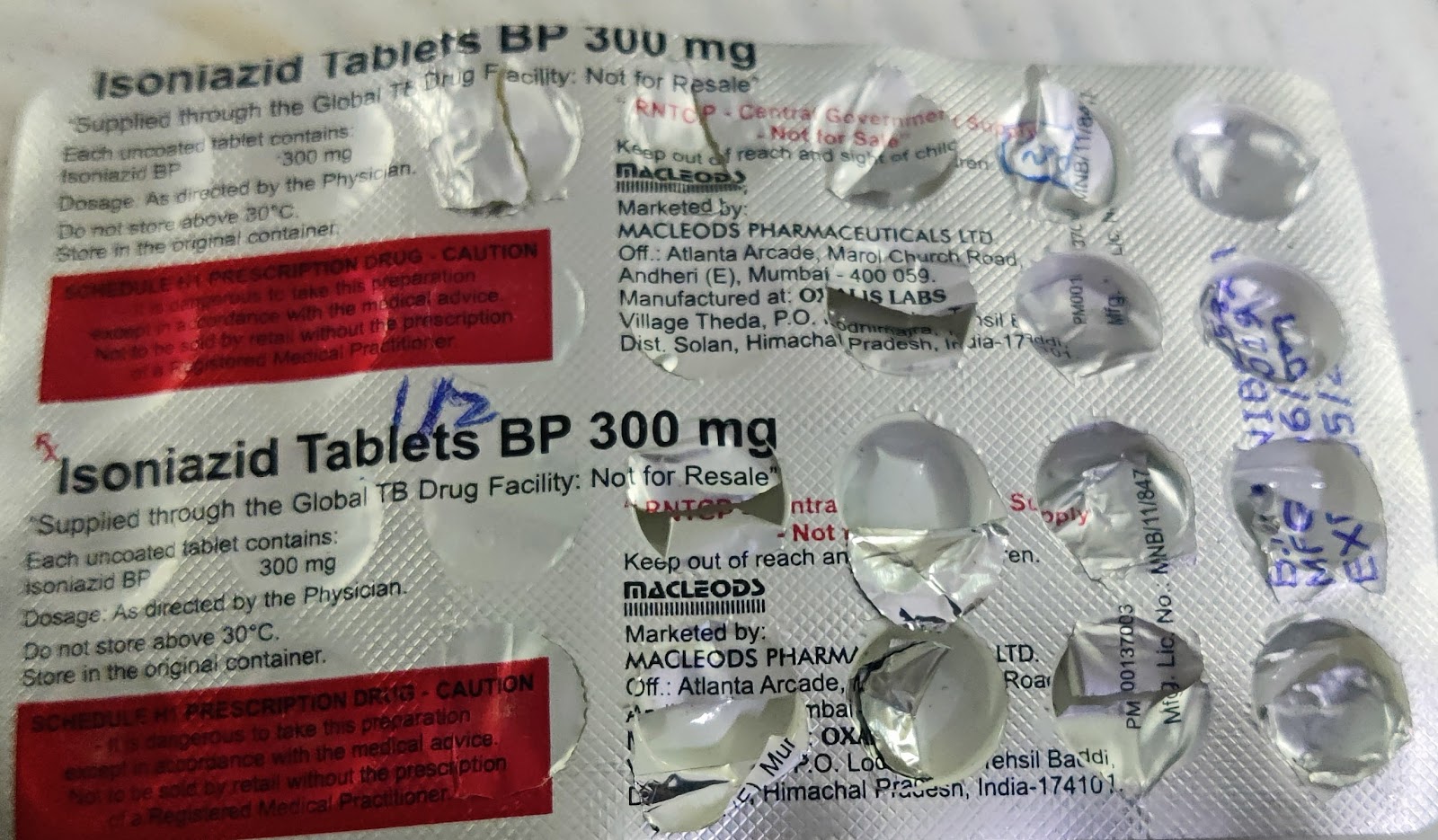
Isoniazid-300mg
Rifampicin-300mg
Pyrazinamide-500mg
Ethambutol -300mg
Ecosprin-75mg
Neurobian forte















Comments
Post a Comment